First-line Helicobacter pylori empirical treatment in the Czech Republic (2019–2024) – initial insights from the European registry on H. pylori management (Hp-EuReg)
Jan Křivinka1, Lumír Kunovský1,2,3, Jitka Vaculová4, Jan Král5,6, Sabina Hrubá7,8, Štěpán Šembera9, Ilja Tachecí9, Petra Čavajdová9, Adam Vašura10, Martin Blaho10, Petra Koňaříková11, Eva Evinová12, Jakub Langner13, Zuzana Vacková14, Pavla Tesaříková15, Natálie Friedová16, Petr Bauer17, David Přidal18, Pavel Sychra19, Anna Cano-Català20, Leticia Moreira21, Pablo Parra22, Francis Mégraud23, Colm O’Morain24, Olga Nyssen22, Javier Gisbert22
+ Affiliation
Summary
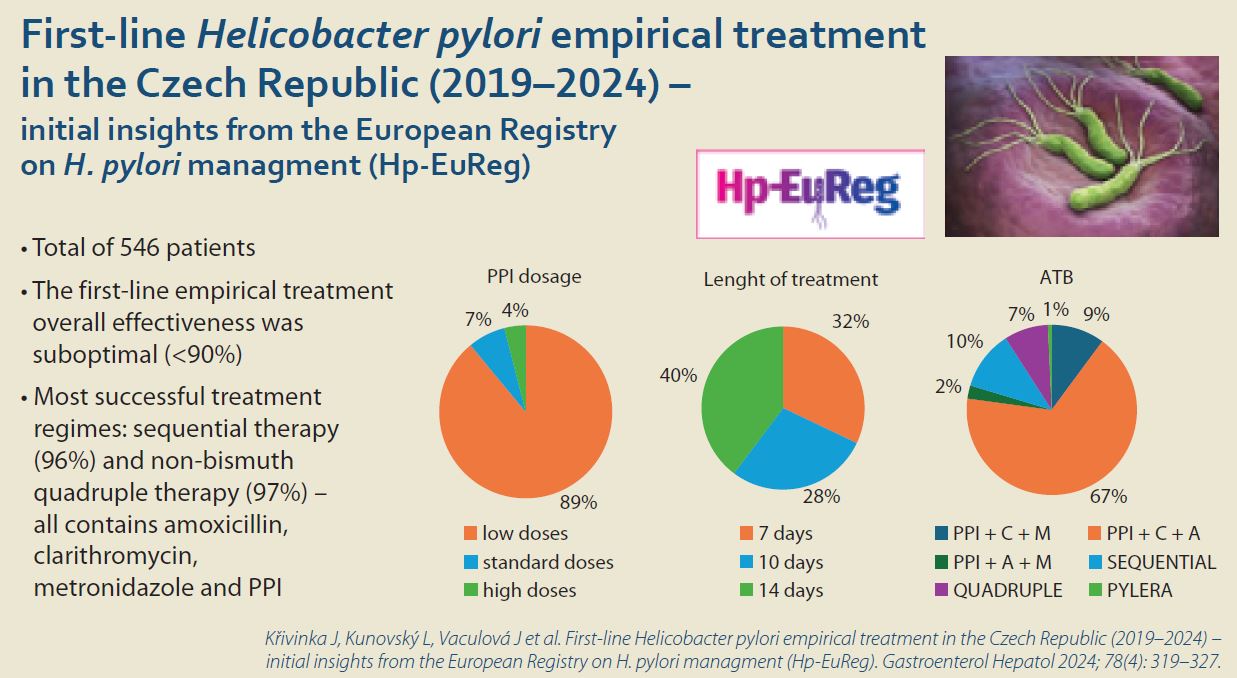
Background and Aim: Helicobacter pylori (H. pylori) infection remains a significant public health concern worldwide, including in the Czech Republic. The study aims to provide an overview of the current first-line treatment approaches for H. pylori infection in the Czech Republic based on data from the European Registry on H. pylori Management (Hp-EuReg), and to evaluate the most effective treatment regimens. Methods: Hp-EuReg is an international multicentric registry on the management of H. pylori, from which we extracted data from the Czech Republic from 2019 to January 2024. This registry collects demographic information, diagnostic procedures, treatment prescriptions, and outcomes for H. pylori infection management by gastroenterologists. A modified intention-to-treat (mITT) analysis was performed to evaluate the effectiveness of the treatments. Results: A total of 546 patients from 14 centres in the Czech Republic who receive first-line treatment were analysed. Low-dose (i.e.; 20 mg omeprazole equivalent twice daily) proton pump inhibitors (PPIs) were administered in 89% of patients, and the most common length of treatments was 14 days (40%). The overall mITT effectiveness of first-line treatment was 85%, obtaining 86% when prescriptions were combined either with low-dose (20 mg omeprazole equivalent twice daily), and high dose (80 mg omeprazole equivalent twice daily) PPIs, and 82.5% with standard-dose (40 mg omeprazole equivalent twice daily) PPIs. The effectiveness of 7-day prescriptions was reported to be 83%, lower than that of 10- and 14-day, both of which achieved effectiveness of 86%. The most frequently used treatment scheme was triple therapy with PPI, amoxicillin and clarithromycin, which was used in 67% of patients, reaching 87% effectiveness both with 7- and 14-day prescriptions. Optimal (>90% mITT) effectiveness was obtained with both 10-day, sequential therapy and with 14-day non-bismuth quadruple concomitant therapy including both PPI, amoxicillin, clarithromycin and metronidazole, providing 96% (48/50 patients) and 97% (34/35 patients) cure rates, respectively. The remaining therapies provided all an effectiveness lower than 90%, the lowest one obtained with PPI, clarithromycin and metronidazole (66%; 35/53 patients). Conclusions: In the Czech Republic, the first-line empirical treatment overall effectiveness was suboptimal (<90%); however, 10-day non-bismuth quadruple sequential and 14-day concomitant therapies, both composed of PPI, amoxicillin, clarithromycin and metronidazole, achieved over 90% cure rates.
Keywords
Helicobacter pylori, first-line treatment, proton pump inhibitors, Czech Republic
Introduction
Helicobacter pylori (H. pylori) is a gram-negative bacterium that can cause several gastrointestinal diseases like atrophic or chronic gastritis, peptic ulcer disease, gastric cancer and mucosa-associated lymphoid tissue (MALT) lymphoma. The infection of H. pylori remains a significant public health concern worldwide, including in the Czech Republic, where the infection prevalence was 23.5% in 2011 [1,2].
Choosing an appropriate treatment regimen is a big challenge in the Czech Republic due to the bacterial antibiotic resistance. Each eradication regimen consists of proton pump inhibitors (PPI), antibiotics and, in some cases, adjuvant bismuth therapy. The effect of PPI is to reduce gastric acidity and increase the pH, which is necessary to eradicate H. pylori effectively. The most widely used regimens in our country are triple therapy (PPI + double combination of antibiotics, usually amoxicillin and clarithromycin), non-bismuth quadruple concomitant therapy (PPI + three antibiotics, usually amoxicillin, clarithromycin and metronidazole), quadruple therapy with bismuth (PPI + bismuth + two antibiotics- metronidazole and tetracycline) and sequential therapy (PPI + one antibiotic for the first half of the regimen and PPI + two antibiotics for the second half of the regimen, usually combination of amoxicillin, clarithromycin and metronidazole) [3]. According to Maastricht VI-Florence consensus [4], in the case of individual bacterial antibiotic sensitivity testing unavailability, the first-line recommended treatment in areas of high (>15%) or unknown clarithromycin resistance is bismuth quadruple therapy (bQT). If this regimen is not available, non-bismuth concomitant quadruple therapy may be considered.
Treatment success rate depends on several factors such as high antimicrobial resistance (the bacterial resistance across all the Europe is 22% for clarithromycin and 27% for metronidazole), [5] the PPI dosage (low, standard or high dose) prescribed and patient compliance (≥90% drug intake) – which depends on several factors such as treatment duration, medication side effects, use of probiotics, receiving sequential or concomitant therapy, rescue treatment, and indicating treatment blindly for unconcluded etiology of dyspepsia or for functional dyspepsia [6].
The aim of this study was to gather information from the European Registry on H. pylori Management (Hp-EuReg) database regarding first-line treatment in the Czech Republic. We analysed the most frequently used eradication treatments to identify the most effective treatment approaches. Our focus included the evaluation of PPI dosage and their effectiveness. Additionally, we compared the cure rates of the three centres with the highest number of registered patients.
Methods
European Registry on Helicobacter pylori Management
This analysis is based on data extracted from the Hp-EuReg, an on-going international, multicentre prospective non-interventionist registry established in 2013 by the European Helicobacter and Microbiota Study Group, covering 38 countries. The registry aims to gather demographic information, treatment diagnoses, prescriptions, previous eradication attempts, and outcomes for managing H. pylori infection. The Czech Republic contributes to this study with 14 participating centres [6].
The study protocol [7] adheres to the ethical guidelines of the 1975 Declaration of Helsinki. It was prospectively registered on ClinicalTrials.gov (NCT02328131) and received approval in 2012 from the Ethics Committee of the Hospital Universitario de La Princesa (Madrid, Spain), serving as the reference Institutional Review Board.
Data management
After data extraction and before statistical analysis, the database underwent a through review for inconsistencies and subsequent data cleaning. The data quality review ensured that study selection criteria were met and that data were correctly collected, adhering to the highest scientific and ethical standards. Discordances in data were resolved through an exhaustive monitoring process by querying investigators and by group emailing.
Anonymized data were collected using an electronic case report form (e-CRF) on the collaborative platform Research Electronic Data Capture (REDCap), hosted by the Asociación Española de Gastroenterología (AEG; www.aegastro.es), a non-profit scientific and medical society dedicated to gastroenterology research, with permission from Vanderbilt University.
Data were extracted in January 2024, focusing on patients receiving first-line treatment in the Czech Republic from 2019 to January 2024. Fol lowing data extraction and before statistical analysis, the database was reviewed for inconsis tencies and cleaned [8].
Study aim
This study aims to evaluate and compare the efficacy and tolerability of first-line treatment regimens for H. pylori infection in a cohort of patients from 14 centres in the Czech Republic. Specifically, the study assessed the effectiveness of commonly prescribed first-line treatments, including triple therapy (PPI + amoxicillin + clarithromycin), sequential therapy and non-bismuth concomitant therapy. It evaluated the occurrence of antibiotic resistance, mainly focusing on clarithromycin and metronidazole resistance, as well as duration of treatment and its impact on treatment effectiveness. Then, the treatment effectiveness in the centres with the highest number of additional patients was compared.
The optimal dosage and duration of PPI therapy required to maximize H. pylori eradication rates while minimizing the risk of recurrence was also investigated.
Statistical analysis
Due to different impacts on the pH of gastric acid, the dosage for individual PPI schedules were recalculated by factors, as reported by Graham et al. [9] and Kirchheiner et al. [10]. PPI dose was calculated in omeprazole equivalents by multiplying the PPI dose for every individually – for the most common used PPI in our region pantoprazole (factor 0.23), 40 mg of pantoprazole is equivalent to 9 mg of omeprazole. Low-dose omeprazole is 4.5–27 mg given twice a day, standard dose is 32–40 mg given twice a day and high-dose is 64–72 mg given twice a day [3,9,10].
The effectiveness of therapy was then analysed using a modified intention-to-treat (mITT), which aims to reflect the closest result to those obtained in clinical practice. It excluded patients uncompliant with the treatment.
Those cases that failed to meet key eligibility criteria or that presented with significant protocol violations that could affect the outcome were excluded.
Adequate treatment compliance was defined as having taken at least 90% of the prescribed treatment drugs. The incidence and type of adverse events (AEs) were also recorded.
Results
Baseline characteristics of the population
Patients were collected across the entire Czech Republic from 14 centres during the period from 2019 to January 2024. Overall, 628 with first-line treatment were registered into the study. This cohort consisted of 54% women (340/628) and 46% men (288/628). Drug allergy occurred in 10% (60/628) of cases, specifically the allergy of penicillin was reported in 8% of patients (50/628). The treatment was most often prescribed for dyspepsia in 56% (353/628), fol lowed by gastric and duodenal ulcers in 22% (138/628) of cases (Tab. 1).
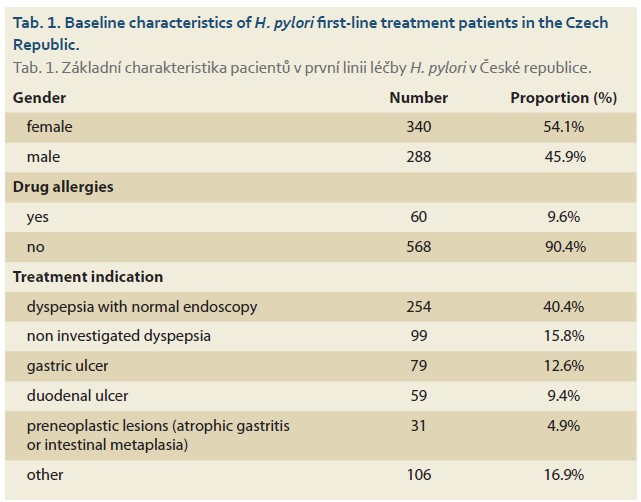
For our study we evaluated 546 patients in the effectiveness analysis.
Prescriptions and effectiveness
The most commonly prescribed treatment for H. pylori was triple therapy, consisting of PPI + amoxicillin + clarithromycin, used in 64% of patients (351 patients) with an effectiveness of 85% regardless of treatment duration and PPI dose.
The effectiveness of treatment according to the duration of therapy was 83%, 86%, and 86% for 7-, 10-, and 14 days, respectively (Tab. 2).
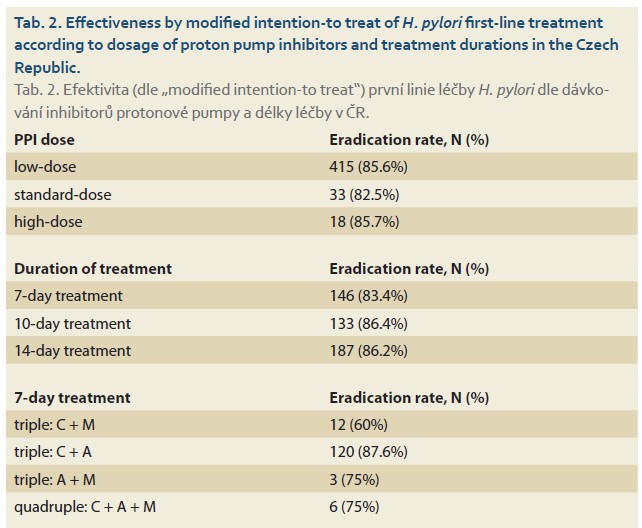
For the 7-day prescriptions, the most successful and most frequent antibiotic combination was PPI + amoxicillin + clarithromycin with an effectiveness of 88% (120/137). The second most prescribed antibiotic combination was PPI + metronidazole + clarithromycin, with a quite suboptimal effectiveness of 60% (12/20). Other eradication treatments were prescribed in fewer than 10 patients.
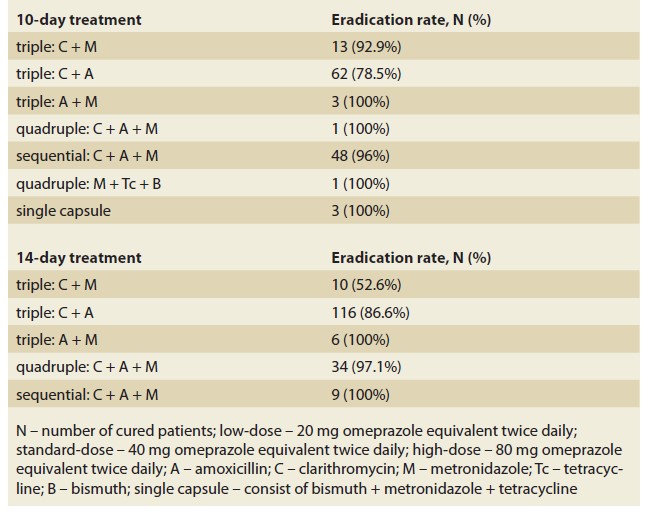
For the 10-day prescriptions, the most commonly used regimen was PPI + amoxicillin + clarithromycin, used in 51% (79/154) of patients, with a reported effectiveness of 79% (62/79), which was again suboptimal. However, the most successful approach for 10-day treatment was sequential therapy with a PPI + amoxicillin + clarithromycin + metronidazole, with an effectiveness of 96% (48/50 patients). This therapy was the second most frequently used in 33% of cases across the 10-day prescriptions (50/154). Another prescribed regimen with more than 10 cases was PPI + metronidazole + clarithromycin with an effectiveness of 93% (13/14).
Regarding 14-day prescriptions, the most prescribed eradication treatment was combination of PPI + amoxicillin + clarithromycin, it was prescribed in 62% of patients in this scheme (134/217) with effectiveness of 87% (116/134). The most successful treatment regimen in this scheme was non-bismuth quadruple concomitant therapy, including PPI + amoxicillin + clarithromycin + metronidazole, which achieved the highest cure rate of 97% (34/35) and was used in 16% of patients in 14-day scheme (35/217). Eradication treatment with suboptimal (<90%) effectiveness was a combination of PPI + metronidazole + clarithromycin with effectiveness of 53% (10/19).
In our cohort, we also evaluated patients according to the PPI dose. Low-dose PPIs were administered in 89% of the patients (485/546) with an effectiveness of 86% (415/485). Standard-dose was prescribed in 7% (40/546) of cases, obtaining a cure rate of 83% (33/40); whereas patients receiving high-dose PPIs was lower in 4% (21/546) reaching a cure rate of 86% (18/21) (Tab. 2).
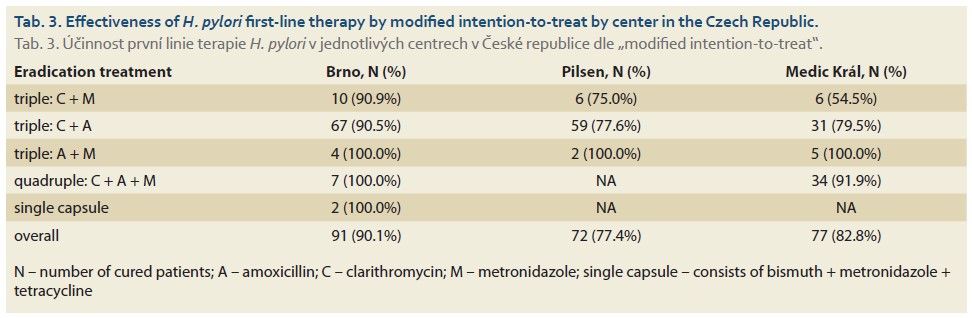
Centres with highest recruitment
We compared three centres with the highest recruitment from across various regions in the Czech Republic: Brno, Pilsen and Medic Král (Prague). In the University Hospital Brno, the most commonly prescribed regimen was a triple therapy consisting of PPI + amoxicillin + clarithromycin with optimal effectiveness of 90%. Overall, the effectiveness in Brno was optimal, and none of the prescribed regimens was below 90% of effectiveness, even the most suboptimal combination of PPI + clarithromycin + metronidazole reported cure rate was over 90%.
In Pilsen, the most frequently used combination was PPI + amoxicillin + metronidazole, whose success rate was 78%, significantly below 90%. The second most prescribed regimen was triple therapy- PPI + clarithromycin + metronidazole with effectiveness of 75%.
In Medic Král (Prague), the most often prescribed regimens were both triple therapies comprising of PPI + amoxicillin + clarithromycin (39 patients) with eradication rate of 79.5% and non-bismuth quadruple concomitant therapy consisting of PPI + amo xicillin + clarithromycin + metronidazole (37 patients) with eradication rate of 92%. Eradication rate of triple therapy, PPI + clarithromycin + metronidazole (11 patients), is noteworthy, reaching only 54.5% in this particular centre (Tab. 3).
Compliance, follow-up and safety
The overall number of patients, who were diagnosed with H. pylori infection and received a first-line treatment, was 628. From those, 13% (81/628) of patients were lost to follow-up, as no confirmation test was performed, and therefore no treatment result was available.
Additionally, 5 patients reported their drug intake was under 90%, but only one of them failed the treatment.
The incidence of at least one AE was reported in 3.2% of patients (20/628). Specifically, these involved dysgeusia (1 patient), diarrhoea (5 patients), nausea (11 patients), vomiting (3 patients), dyspepsia (4 patients) and abdominal pain (1 patient).
Discussion
In our study on the H. pylori first-line treatment regimens in the Czech Republic between years 2019 and 2024, we investigated the most commonly prescribed empirical regimens, assessed their effectiveness, by analysing the prescribed PPI dosages and therapy durations. The management of the infection was also compared among recruiting centres.
By far, the most prescribed first-line eradication treatment regimen in the Czech Republic was triple therapy of PPI + amoxicillin + clarithromycin. This treatment was used in 64% of included patients, six times more often than the second most prescribed treatment regimen- sequential therapy (PPI + amoxicillin + clarithromycin + metronidazole), prescribed in 11% of patients. This triple therapy (PPI + amoxicillin + clarithromycin) has an overall effectiveness of 85% independent of treatment duration and PPI dose. The effectiveness, nevertheless, was below the arbitrary threshold for acceptance of the proposed treatment (<90% eradication rate) [4]. If we take a look at treatment duration, no significant difference between 7-, 10- and 14-day regimens was reported. No significant differences were observed even if PPI dose was specifically compared for the triple therapy of PPI + amoxicillin + clarithromycin. Comparing our findings for the triple therapy with those reported by Nyssen et al. in 2020, who evaluated eradication treatments regimens across Europe over 5-year period, similar results were observed for PPI + amoxicillin + clarithromycin therapy, with effectiveness rates of 83%, 84%, and 86% for 7-days, 10-days, and 14-days of treatment, respectively [11]. The exact same results were reported in the Czech Republic for this therapy, in line with the overall assessment findings encompassing all European countries. The most significant difference was in the 10-day treatment of PPI + amoxicillin + clarithromycin, likely due to high clarithromycin resistance in certain areas. Specifically in Pilsen, the effectiveness of this therapy (PPI + amoxicillin + clarithromycin) was only 47% (7/15) for a 10-day regimen.
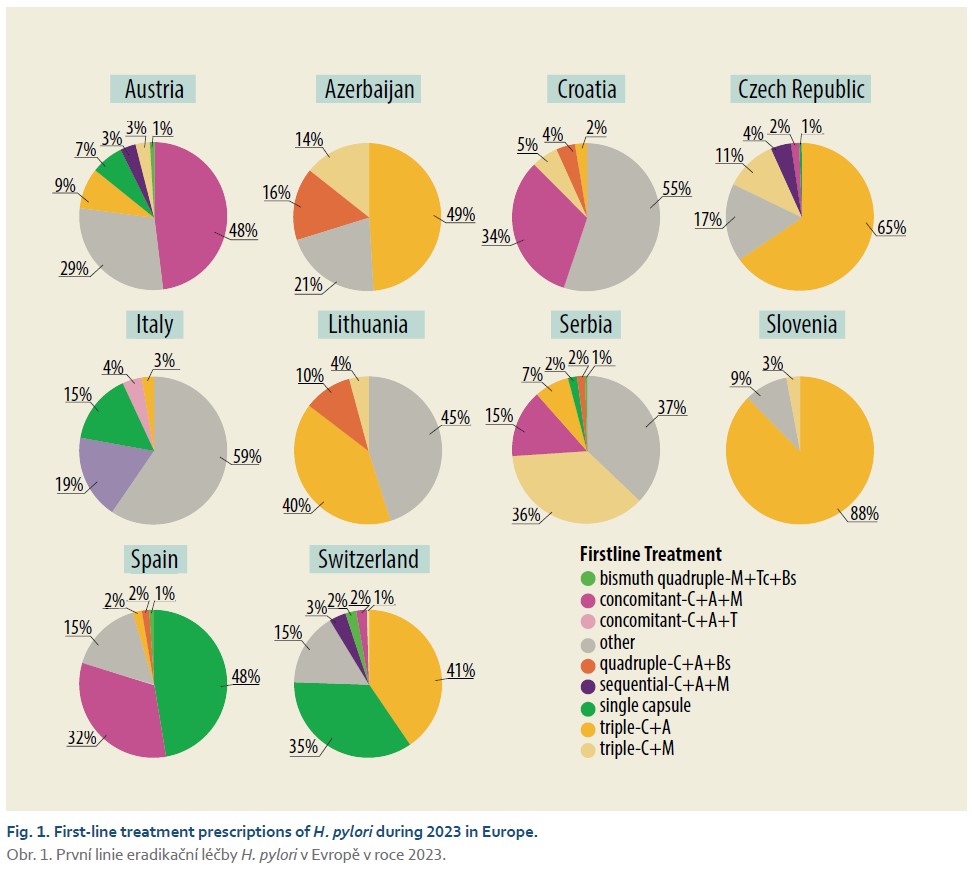
Comparing eradication regimens across Europe with our results and eradication strategy, we observed both similarities and differences in the choice of the first-line empirical treatment. According to the attached pie chart (Fig. 1) [12], the most frequently prescribed eradication regimen during the 2023 year in the Czech Republic, Azerbaijan, Lithuania, Switzerland, and Slovenia was a combination of PPI + amoxicillin + clarithromycin. Evaluating the study by Tepes [13] from Slovenia (2017–2019), it shows a higher cure rate with this same triple therapy regimen lasting 14 days with a 93% (714 patients) success rate compared to our cure rate of 87% (134 patients). This difference is likely attributed to a lower antibiotic resistance prevalence to clarithromycin in Slovenia, which is currently below 15%. In contrast, the Czech Republic has higher clarithromycin resistance, potentially necessitating a revised strategy for prescribing eradication regimens in certain regions. One alternative could be the bismuth quadruple therapy prescribed as a three-in-one capsule (marketed Pylera®) containing bismuth, tetracycline and metronidazole, which is prescribed in 48% of cases in Spain and 35% in Switzerland, a stark contrast to the Czech Republic, where Pylera® was prescribed as a first-line drug in only four cases, who were successfully cured. Nevertheless, it should be noted that this three-in-one capsule bismuth quadruple therapy has not been covered by the health insurance in the Czech Republic since 2020 and has only been available through import from other countries.
Also, comparing the results for triple therapy of PPI + amoxicillin + clarithromycin in our three centres with the highest recruitment- Brno, Pilsen and Medic Král (Prague). There were noted significant differences in the success of H. pylori eradication among these centres. The most successful centre with this particular therapy was University Hospital Brno, which achieved approximately 90% overall effectiveness. We can estimate the antibiotic resistance to clarithromycin is <15% in Brno.
On the other hand, the centres in Pilsen and Prague had an overall effectiveness of 78% and 79,5%, respectively. This discrepancy may be attributed to higher resistance to clarithromycin in these regions, because when we look at other combination with clarithromycin in these centres, triple therapy of PPI + clarithromycin + metronidazole presented similar discouraging results. In Pilsen, the same triple therapy achieved a 75% eradication rate, and Medic Král reported 54.5% effectiveness. In contrast, Brno achieved a successful rate of 91%, which is similar to other triple therapy combining PPI + amoxicillin + clarithromycin. Another crucial factor for successful therapy is the duration of treatment. In each centre (Brno, Pilsen, Medic Král), there was a notice able increase in effectiveness with longer therapy durations. Specifically, in Pilsen, we observed that longer duration of treatment led to higher effectiveness. For a 7-day treatment, the effectiveness was 50% (1/2 patients); for a 10-day treatment, it was 47% (7/15 patients); and for a 14-day treatment, it rose to 86% (51/59 patients).
A solution to increase the success rate of eradication in Pilsen and Medic Král (Prague) could be to change the strategy of therapy, considering the high failure rate observed when using clarithromycin-containing therapy. Results from our study show that it may be beneficial to start prioritizing a 10-day sequential therapy prescription (PPI + amoxicillin for 5 days, combination of PPI + clarithromycin + metronidazole for another 5 days), which reported an optimal eradication rate of 96%. Another option could be a non-bismuth quadruple concomitant therapy used for 14 days with even higher eradication rate of 97%. To confirm the statement about the need of strategy change- the switch from triple therapy of PPI + amoxicillin + clarithromycin to a non-bismuth quadruple concomitant therapy- we provide an example as fol lows. In Medic Král (Prague), triple therapy was prescribed for 39 patients and quadruple therapy for 37 ones with different results. Triple therapy presented with the eradication rate of only 79%. However, when prescribed with quadruple therapy, the eradication rate was much higher – 92%, which is over the optimal 90% threshold.
Another option for centres with low eradication success rates using clarithromycin containing regimens could be a single capsule containing bismuth, tetracycline and metronidazole. The patient takes 12 pills a day (divided into three or four intakes) in combination with PPI taken twice a day. According to data from the study by Nyssen et al., in which they collected 2,100 patients, the eradication rate of single capsule was 95% if used as first-line treatment, for the second line 89% and for a rescue therapy the eradication rate was 92% [14]. These are promising digits of the eradication rate. In another study by Nyssen et al., eradication regimens for patients with penicillin allergy were examined, comparing the effectiveness of PPI + clarithromycin + metronidazole (69%) against PPI + bismuth + metronidazole + tetracycline (91%) as first-line treatments [15]. In the Czech Republic, the combination of PPI + clarithromycin + metronidazole is the most prescribed regimen for patients with penicillin allergy, with an overall effectiveness of 66% (35/53 patients), similar to the effectiveness reported by a study by Nyssen et al. We can estimate that using a single capsule could be the solution for patients with penicillin allergy, potentially increasing the eradication success rate. From the beginning of July 2024, the single capsule Pylera® will be available for prescription in the Czech Republic. Indication criteria for prescription of Pylera® in the Czech Republic are allergy of amoxicillin or failure of first-line treatment or any of rescue treatment [8,14,15].
In the Czech Republic, a higher eradication rate could be reached by increasing the PPI dose. According to our results, most of the eradication treatment regimens were underdosed concerning the PPI. Low-dose option was prescribed in 89% of patients as the first-line. That could be due to wrong choice of PPI and their inappropriate dose, failing to reach an optimal pH of acid in stomach. In our country, the most commonly used PPI is pantoprazole, which was proven to have insufficient influence on stomach pH, according to studies by Graham and Kirchheiner. Pantoprazole has a factor of 0.23 compared to omeprazole, meaning that, for example, 40 mg of pantoprazole is equivalent to only 9 mg of omeprazole [3,9,10]. Switching to omeprazole could be a solution to increase the overall eradication rate in the Czech Republic, or the maximum dose of pantoprazole – 80 mg prescribed twice a day. On the other hand, we didn’t find a significant difference between PPI doses: the effectiveness was 86% for the low-dose, 83% for the standard-dose and 86% for high-dose regimens. This could be due to low number of total enrolled patients. In the study by Pabón-Carrasco et al. [8], standard or high-dose regimens are recommended for the first-line treatment. In their research, high-dose PPIs in 14-day triple therapy and 10- or 14-day quadruple concomitant therapy are recommended, while standard-dose PPIs would be sufficient in 10-day bismuth quadruple therapy.
Our study has some limitations. One is a small sample size, enrolling only 546 patients who received a first-line treatment during the period of 5 years. Additionally, two of our three centres with the highest patient enrolment likely have high clarithromycin resis tance. We can’t estimate the clarithromycin resis tance in other centres because of an insufficient set of patients.
In the Czech Republic, optimal (>90%) first-line empirical treatment effectiveness was achieved with a 10-day non-bismuth quadruple sequential therapy (PPI + amoxicillin + clarithromycin + metronidazole) and a 14-day non-bismuth concomitant therapy (PPI + amoxicillin + clarithromycin + metronidazole). The overall first-line treatments’ effectiveness in the Czech Republic was 85%, which was below the desired 90% threshold of eradication success rate, which could be explained by the high bacterial clarithromycin resistance in our setting and/or by the frequent use of 7-day regimens and low-dose PPI regimens.
Author’s contribution:
Jan Křivinka, planned and coordinated the study; extracted, analysed, synthetized and interpreted the data; wrote the first draft and approved the submitted manuscript.
Lumír Kunovský collected the data, critically reviewed the manuscript’s drafts, and approved the final submitted manuscript.
Jitka Vaculová, Jan Král, Sabina Hrubá, Štěpán Šembera, Ilja Tachecí, Petra Čavajdová, Adam Vašura, Martin Blaho, Petra Koňaříková, Eva Evinová, Jakub Langner, Zuzana Vacková, Petra Tesaříková, Natálie Friedová, Petr Bauer, David Přidal and Pavel Sychra enrolled patients in Hp-EuReg at their centers.
Anna Cano and Pablo Parra, performed the monitoring and quality check of the data, and approved the final manuscript.
Olga P. Nyssen, Hp-EuReg Scientific Director, performed the data extraction, supervised the monitoring and quality check, assisted with data interpretation and synthesis, critically reviewed the manuscript’s drafts and approved the final submitted manuscript.
Pablo Parra, Anna Cano-Català, Leticia Moreira, Olga P. Nyssen, Francis Megraud, Colm O Morain, Javier P. Gisbert are all members of the Hp-EuReg Scientific Committee; they critically reviewed the manuscript’s drafts, and approved the final submitted manuscript.
Javier P. Gisbert, Principal investigator of the registry, directed the project, obtained funding, designed the protocol, recruited patients, critically reviewed the manuscript drafts, and approved the final submitted manuscript.
Acknowledgements
We thank the Spanish Association of Gastroenterology (AEG) for providing the e-CRF service free of charge.
ORCID authors
J. Křivinka 0009-0008-2705-1357,
L. Kunovský 0000-0003-2985-8759,
J. Král 0000-0001-6960-1013,
Š. Šembera 0000-0003-0151-9982,
P. Čavajdová 0009-0003-9447-1515,
A. Vašura 0000-0001-9289-6198,
J. Langner 0009-0009-9570-4468,
Z. Vacková 0000-0002-0443-5752,
N. Friedová 0000-0003-3482-0878,
P. Bauer 0009-0009-9362-3488,
J. P. Gisbert 0000-0003-2090-3445.
Submitted/Doručeno: 7. 8. 2024
Accepted/Přijato: 12. 8. 2024
Corresponding author
Assoc. Prof. Lumír Kunovský, MD, PhD
2nd Department of Internal Medicine – Gastroenterology and Geriatrics,
University Hospital Olomouc,
Faculty of Medicine and Dentistry,Palacky University Olomouc
Zdravotníků 248/7
779 00 Olomouc
Czech Republic
lumir.kunovsky@fnol.cz
To read this article in full, please register for free on this website.
Benefits for subscribers
Benefits for logged users
Literature
1. Milivojevic V, Babic I, Kekic D et al. Current trends in the management of Helicobacter pylori infection in Serbia: preliminary results from the European registry on H. pylori man agement. Dig Dis 2022; 41(3): 377–386. doi: 10.1159/000528389.
2. Bureš J. Significant decrease in prevalence of Helicobacter pylori in the Czech Republic. World J Gastroenterol 2012; 18(32): 4412–4418. doi: 10.3748/wjg.v18.i32.4412.
3. Pérez-Aisa Á, Nyssen OP, Keco-Huerga A et al. Bismuth quadruple three-in-one single capsule three times a day increases effectiveness compared with the usual four times a day schedule: results from the European registry on Helicobacter pylori management (Hp-EuReg). Gut 2023; 72(11): 2031–2038. doi: 10.1136/gutjnl-2022-329259.
4. Malfertheiner P, Megraud F, Rokkas T et al. Management of Helicobacter pylori infection: the Maastricht VI/Florence consensus report. Gut 2022; 71(9): 1724–1762. doi: 10.1136/gutjnl-2022-327745.
5. Bujanda L, Nyssen OP, Ramos J et al. Effectiveness of Helicobacter pylori treatments according to antibio tic resistance. Am J Gastroenterol 2024; 119(4): 646–654. doi: 10.14309/ajg.000 0000000002600.
6. Huguet JM, Ferrer‐Barceló L, Suárez P et al. Role of compliance in Helicobacter pylori eradication treatment: results of the European registry on H. pylori management. United European Gastroenterol J 2024; 12(6): 691–704. doi: 10.1002/ueg2.12569.
7. McNicholl AG, O’Morain CA, Megraud F et al. Protocol of the European registry on the management of Helicobacter pylori infection (Hp‐EuReg). Helicobacter 2019; 24(5): e12630. doi: 10.1111/hel.12630.
8. Pabón‐Carrasco M, Keco‐Huerga A, Castro‐Fernández M et al. Role of proton pump inhibitors dosage and duration in Helicobacter pylori eradication treatment: results from the European registry on H. pylori management. United European Gastroenterol J 2024; 12(1): 122–138. doi: 10.1002/ueg2.12476.
9. Graham DY, Lew GM, Malaty HM et al. Factors influencing the eradication of Helicobacter pylori with triple therapy. Gastroenterology 1992; 102(2): 493–496. doi: 10.1016/0016-5085(92)90095- g.
10. Kirchheiner J, Glatt S, Fuhr U et al. Relative potency of proton-pump inhibitors – comparison of effects on intragastric pH. Eur J Clin Pharmacol 2009; 65(1): 19–31. doi: 10.1007/s00228-008-0576-5.
11. Nyssen OP, Bordin D, Tepes B et al. European registry on Helicobacter pylori management (Hp-EuReg): patterns and trends in first-line empirical eradication prescription and outcomes of 5 years and 21 533 patients. Gut 2021; 70(1): 40–54). doi: 10.1136/gutjnl-2020-321372.
12. European registry on the management of Helicobacter pylori infection. 2024 [online]. Available from: https: //www.aegastro.es/hpeureg.
13. Tepes B, Brglez Jurecic N, Tepes K et al. Helicobacter pylori: eradication rates in Slovenia in the period from 2017 to 2019: data from the European registry on H. pylori management. Dig Dis 2021; 39(4): 318–324. doi: 10.1159/000512506.
14. Nyssen OP, Perez‐Aisa A, Castro‐Fernandez Met al. European registry on Helicobacter pylori management: single‐capsule bismuth quadruple therapy is effective in real‐world clinical practice. United European Gastroenterol J 2021; 9(1): 38–46. doi: 10.1177/2050640620972615.
15. Nyssen OP, Pérez‐Aisa Á, Tepes B et al. Helicobacter pylori first‐line and rescue treatments in patients allergic to penicillin: experience from the European registry onH pylorimanagement (Hp‐EuReg). Helicobacter 2020; 25(3): e12686. doi: 10.1111/hel.12686.